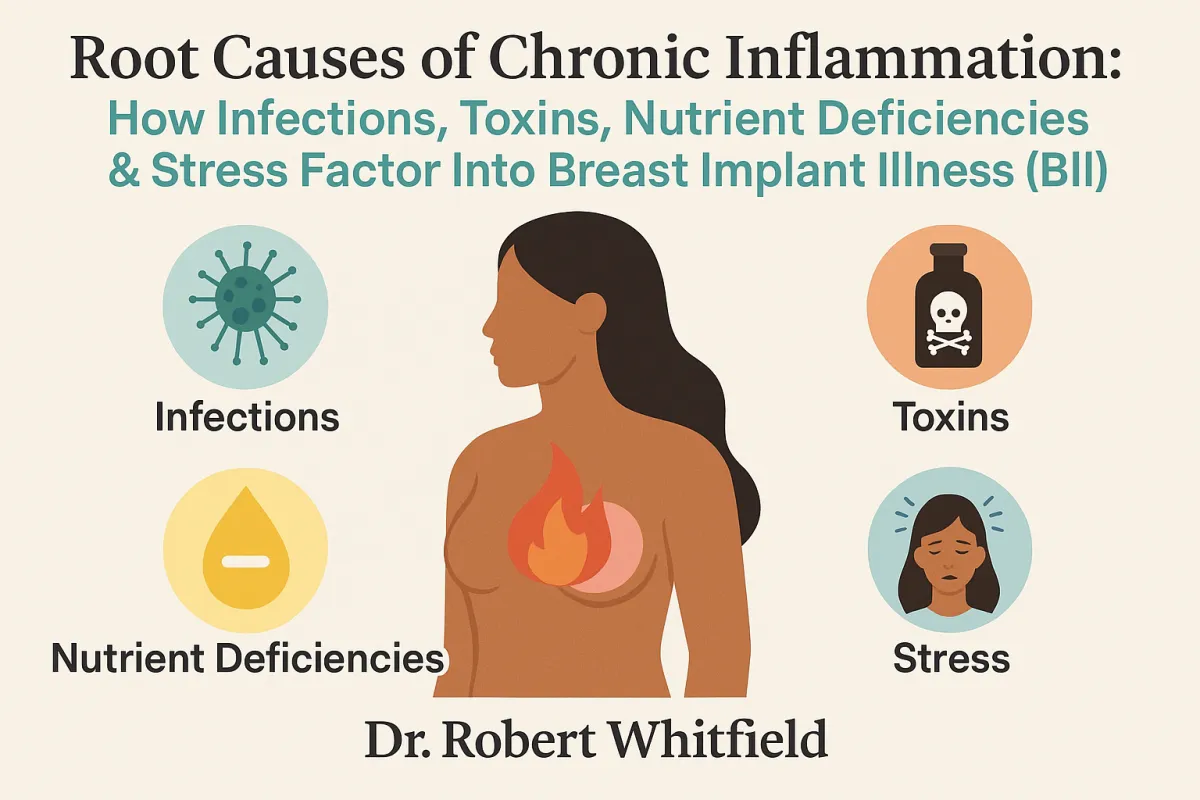
Root Causes of Chronic Inflammation: How Infections, Toxins, Nutrient Deficiencies & Stress Factor Into Breast Implant Illness (BII)
Root Causes of Chronic Inflammation: How Infections, Toxins, Nutrient Deficiencies & Stress Factor Into Breast Implant Illness (BII)
Breast implant illness (BII) is a collection of symptoms that some women with breast implants experience. These symptoms can include fatigue, brain fog, joint pain, hair loss, headaches, and digestive issues, among others. While BII is not an official medical diagnosis, more and more women are reporting these troubling symptoms to their doctors.
So, what exactly causes breast implant illness? While the precise mechanisms are still being researched, four key factors are thought to drive the chronic inflammation at the root of BII symptoms: infections, toxins, nutrient deficiencies, and stress.
Let's take a closer look at each of these factors.
1. Infections
Studies have found that the scar tissue capsules that form around breast implants can harbor bacteria [1]. This bacterial contamination may trigger an immune response and systemic inflammation. In fact, one study found that 29% of explant scar capsules tested positive for bacterial contamination [2].
The most common culprits were Cutibacterium acnes (formerly Propionibacterium acnes) and Staphylococcus epidermidis [2]. Interestingly, these are not the types of acute infections that would typically cause redness, swelling, and fever. Rather, they are slow-growing, low-virulence microbes that can persist undetected for years, causing low-grade inflammation and/or minor symptoms like acne [3].
However, they’re not the only kinds of infections that can lead to inflammation. Infections in the gut microbiome can also contribute to the systemic inflammation we see in BII. Gut dysbiosis, characterized by an overgrowth of harmful microbes, can lead to increased intestinal permeability or "leaky gut," which allows toxins and bacteria to enter the bloodstream, triggering a chronic immune response [4, 5]. This gut-derived inflammation, combined with the low-grade infections around breast implants and exposure to environmental toxins, can contribute to the total toxic load on the body. When this burden exceeds an individual's threshold, the diverse symptoms of BII can appear.
2. Toxins
We are exposed to countless toxins every day – in the air we breathe, the water we drink, the food we eat, and the products we use.
Some common toxins include:
Mold toxins
Exposure to toxic mold from water-damaged buildings is surprisingly common. In fact, a 2022 study from National Institute for Occupational Safety and Health Centers for Disease Control and Prevention (NIOSH) estimates that nearly half of all buildings in America (47%) have mold [6]. Mold can also grow on crops in the field or during storage, and may not always be visible. Ingesting even small amounts of mycotoxins over time can lead to toxic buildup. Mold toxins can cause neurological symptoms, hormonal imbalances, and immune dysfunction.
Heavy metals
Heavy metals like mercury, lead, cadmium, and arsenic can accumulate in the body over time. We can be exposed to heavy metals through dental fillings, contaminated seafood, old lead paint, and polluted air or water. They are neurotoxic and can impair detoxification pathways, leading to symptoms like fatigue, brain fog, and digestive issues.
Pesticides and herbicides
Residues from pesticides and herbicides used in conventional agriculture can disrupt hormones and damage the gut lining. These chemicals are not just found on the surface of produce. They are absorbed into the plant tissues and can also contaminate soil and groundwater, making them nearly impossible to avoid completely.
Plasticizers
Chemicals used to make plastics soft and flexible (like BPA and phthalates) are known endocrine disruptors. They can leach from food packaging and alter hormone function, leading to symptoms like weight gain, reproductive issues, and increased risk of certain cancers.
PFAS chemicals
Per- and polyfluoroalkyl substances (PFAS) are used to make non-stick cookware, stain-resistant fabrics, and waterproof clothing. They are known as "forever chemicals" because they do not break down in the environment and can accumulate in the body over time. PFAS exposure has been linked to immune dysfunction, thyroid disorders, and certain cancers.
VOCs
Volatile organic compounds (VOCs) are found in paint, new furniture, carpeting, and many cleaning products. They can off-gas into the air and be inhaled, causing respiratory irritation, headaches, and dizziness. Some VOCs, like formaldehyde, are known carcinogens.
Personal care products
The average woman uses 13 personal care products per day, exposing her to 114 unique chemicals; for men, it’s about 11 products and 105 chemicals. [7] Many of these chemicals, like parabens and triclosan, are known endocrine disruptors that can mimic or block hormone function. You’re likely to find these chemicals in products such as shampoos, conditioners, lotions, cosmetics, toothpastes, and deodorants.
Internal toxins
Not all toxins come from our external environment. Our bodies also produce toxic byproducts as a result of normal cellular processes, such as metabolic waste and oxidative stress. While our detoxification systems are designed to handle these endogenous toxins, the sheer volume of environmental toxins we now face can overwhelm our natural cleaning capacity.
When our bodies are overburdened with toxins, it can lead to chronic inflammation and oxidative stress. Breast implants may act as a "tipping point" for women who already have high toxic body burdens. The additional foreign material and potential for microbial contamination could overwhelm an already taxed system [8].
Some people also have genetic variations that impair their ability to detoxify properly. If your detoxification pathways are sluggish, you may not be able to efficiently clear toxins, leading them to recirculate and cause damage.
3. Nutrient Deficiencies
Nutrient deficiencies are common in today's world of processed, nutrient-poor foods. Deficiencies in key anti-inflammatory nutrients like omega-3 fatty acids, vitamin D, and magnesium can allow inflammation to run unchecked [9].
Breast implants may exacerbate nutrient deficiencies in several ways:
Malabsorption: If breast implants contribute to gut dysbiosis and intestinal permeability, it can impair the absorption of nutrients from food.
Increased nutrient demands: The body requires extra nutrients to mount an immune response and deal with the added burden of a foreign object.
Appetite changes: Some women with BII report changes in appetite and food cravings, which may alter their nutrient intake.
Correcting nutrient deficiencies through a nutrient-dense diet and targeted supplementation can help quell inflammation and support healing.
However, before blindly adding nutrients, finding out exactly what your body is missing is crucial. This can be accomplished by conducting comprehensive nutritional testing, such as an organic acids test (OAT), which can pinpoint specific deficiencies. An OAT measures levels of key vitamins, minerals, amino acids, and fatty acids. However, it's best to address any gut infections or permeability issues before doing an OAT to ensure accurate results.
4. Stress
Chronic psychological stress keeps the body in "fight or flight" mode, fueling inflammation. It also degrades the gut lining and alters the microbiome [10].
Stress triggers the release of cortisol and other inflammatory cytokines. Chronic elevations of these chemicals can lead to widespread inflammation and immune dysregulation.
For many women, the decision to get breast implants is fraught with emotional factors like body image concerns, relationship issues, and societal pressure. The surgery and recovery period can also be stressful, both physically and emotionally.
Furthermore, dealing with mysterious symptoms and struggling to find answers can be incredibly stressful for women with BII. The lack of mainstream medical recognition and limited treatment options can leave women feeling dismissed and hopeless.
Studies have shown that emotional and social support can significantly impact healing outcomes. One study found that patients with strong social support networks had better physical and mental health outcomes following surgery compared to those with less support [11]. Another study demonstrated that patients who received emotional support and stress management interventions before and after surgery had reduced inflammation, better wound healing, and shorter hospital stays [12].
That’s why we take a mind-body-spirit approach with our patients, including mental/emotional support strategies in addition to physical treatments. Managing stress through techniques like meditation, deep breathing, therapy, and social support is crucial for rebalancing the immune system and promoting healing.
The Problem with Detoxing Too Soon
If you suspect breast implants are contributing to your health issues, you may be tempted to jump right into a detox protocol – things like juice cleanses, liver flushes, or chelation therapy. However, this can actually make you feel worse if your drainage pathways are not open and functioning properly.
Drainage pathways refer to the routes through which your body eliminates toxins and waste products, primarily the liver, kidneys, intestines, skin, and lymphatic system. If these pathways are overburdened or blocked, toxins can't efficiently exit the body. Trying to detox without first opening drainage pathways is like stirring up debris in a stagnant pond – it just swirls around and settles back down, making the water more murky.
A common example of this is the Herxheimer reaction, or "die-off" reaction. This occurs when large quantities of toxins are released into the system too quickly, leading to a temporary worsening of symptoms. Flu-like symptoms, headaches, brain fog, and skin rashes are common Herxheimer manifestations as the body struggles to eliminate the sudden influx of toxins.
Supporting Drainage Pathways
Before embarking on any detox protocol, it's essential to gently open and support your body's innate drainage pathways. This will prevent detox reactions and ensure toxins have a clear exit route as they are mobilized from tissues.
Here are some ways to stimulate drainage:
Poop every day: Many toxins are expelled through solid waste. Constipation allows toxins to be reabsorbed into the bloodstream instead of being eliminated. Aim for at least one fully evacuated bowel movement daily.
Fiber: Eating plenty of fiber from fruits, vegetables, and whole grains keeps things moving through the digestive tract and binds to toxins for elimination.
Hydration: Drinking enough clean, filtered water is essential for flushing toxins out through the kidneys and colon.
Support your gut microbiome: A healthy balance of beneficial bacteria helps keep pathogens in check, regulates inflammation, and maintains intestinal barrier function. Fermented foods and a diverse plant-based diet can support your microbiome. If using probiotics, start slow and work with a practitioner to ensure you are addressing any underlying dysbiosis first.
Stimulate lymphatic flow: Your lymphatic system collects cellular waste and toxins from tissues and transports them to the bloodstream for elimination. Unlike blood, lymph does not have a pump and relies on movement to flow. Dry brushing, rebounding, or lymphatic drainage massage can help mobilize stagnant lymph.
Support your liver: As your main detoxification organ, your liver works hard to break down toxins and prepare them for elimination. Eating liver-supportive foods like cruciferous vegetables, garlic and beets, and taking supplements like milk thistle and glutathione can enhance the liver's natural detox capacity.
Movement: Exercise and deep breathing stimulate lymphatic flow and help pump toxins out through the lungs and skin.
Reduce overall inflammation: Chronic inflammation impairs detoxification and overburdens drainage pathways. Key nutrients for lowering inflammation include omega-3 fatty acids, curcumin, resveratrol, and quercetin. We also recommend supporting the body with liposomals for Vitamin B, Vitamin C, Vitamin D, glutathione, carnitine, and magnesium, which work together to support the body's natural anti-inflammatory processes, boost immune function, and promote cellular repair. Liposomal delivery is crucial because it protects these nutrients from breakdown in the digestive tract, allowing for better absorption and bioavailability. This means that more of the active compounds can reach the cells where they are needed most. Check out our Inflammation Support Bundle, which has all the key liposomals you need for lowering inflammation to support your natural healing abilities.
Once drainage pathways are functioning well, you can slowly add in additional detox support like infrared sauna, chelation therapy, or coffee enemas with the guidance of an experienced practitioner. These therapies can help mobilize toxins from tissues and enhance elimination, but only if the body is able to handle the increased toxic load. Starting too aggressive a detox protocol without adequate drainage support is a recipe for severe detox reactions.
Putting the Pieces Together
Breast implant illness is a complex condition with multiple contributing factors, including infections, toxins, nutrient deficiencies, and stress. These factors combine to create a perfect storm of chronic inflammation and immune dysfunction.
To fully recover from breast implant illness, it's crucial to address the root causes and imbalances that allowed symptoms to arise in the first place. This often requires a comprehensive approach involving:
Identifying and treating any infections
Reducing toxic burden through lifestyle upgrades
Correcting nutrient deficiencies
Managing stress
Supporting drainage pathways BEFORE detoxing
Potential explant surgery to remove the source of inflammation
Working with a practitioner who understands the complexities of breast implant illness and can create a personalized treatment plan is paramount. With patience, persistence, and the right interventions, many women are able to reclaim their health and vitality.
Remember, you are your own best advocate. Keep searching for answers, trust your intuition, and don't give up hope. Healing is possible.
To your health,
Dr. Robert Whitfield
References
[1] Gorgy, A., Barone, N., Nepon, H., Dalfen, J., Efanov, J. I., Davison, P., & Vorstenbosch, J. (2023). Implant-based breast surgery and capsular formation: when, how and why?—a narrative review. Annals of Translational Medicine, 11(11), 385. https://doi.org/10.21037/atm-23-131
[2] Whitfield, R., Tipton, C. D., Diaz, N., Ancira, J., & Landry, K. S. (2024). Clinical Evaluation of Microbial Communities and Associated Biofilms with Breast Augmentation Failure. Microorganisms, 12(9), 1830. https://doi.org/10.3390/microorganisms12091830
[3] Rieger, U. M., Mesina, J., Kalbermatten, D. F., Haug, M., Frey, H. P., Pico, R., Frei, R., Pierer, G., Lüscher, N. J., & Trampuz, A. (2013). Bacterial biofilms and capsular contracture in patients with breast implants. British Journal of Surgery, 100(6), 768–774. https://doi.org/10.1002/bjs.9084
[4] Kho, Z. Y., & Lal, S. K. (2018). The human gut microbiome – a potential controller of wellness and disease. Frontiers in Microbiology, 9. https://doi.org/10.3389/fmicb.2018.01835
[5] Arrieta, M. C. (2006). Alterations in intestinal permeability. Gut, 55(10), 1512–1520. https://doi.org/10.1136/gut.2005.085373
[6] Park, J., & Cox-Ganser, J. (2022). NIOSH Dampness and Mold Assessment Tool (DMAT): Documentation and data analysis of Dampness and Mold-Related Damage in Buildings and its application. Buildings, 12(8), 1075. https://doi.org/10.3390/buildings12081075
[7] Survey finds use of personal care products up since 2004 – what that means for your health. (2023, July 26). Environmental Working Group. https://www.ewg.org/research/survey-finds-use-personal-care-products-2004-what-means-your-health
[8] Lee, M., Ponraja, G., McLeod, K., & Chong, S. (2020). Breast Implant Illness: A Biofilm hypothesis. Plastic & Reconstructive Surgery Global Open, 8(4), e2755. https://doi.org/10.1097/gox.0000000000002755
[9] Ruiz-Núñez, B., Pruimboom, L., Dijck-Brouwer, D. J., & Muskiet, F. A. (2013). Lifestyle and nutritional imbalances associated with Western diseases: causes and consequences of chronic systemic low-grade inflammation in an evolutionary context. The Journal of Nutritional Biochemistry, 24(7), 1183–1201. https://doi.org/10.1016/j.jnutbio.2013.02.009
[10] Madison, A. A., & Bailey, M. T. (2023). Link Stress-Related gut microbiota shifts to mental health outcomes. Biological Psychiatry, 95(4), 339–347. https://doi.org/10.1016/j.biopsych.2023.10.014
[11] Drageset, J. (2021). Social support. In Springer eBooks (pp. 137–144). https://doi.org/10.1007/978-3-030-63135-2_11
[12] Gouin, J., & Kiecolt-Glaser, J. K. (2010). The impact of psychological stress on wound healing: Methods and mechanisms. Immunology and Allergy Clinics of North America, 31(1), 81–93. https://doi.org/10.1016/j.iac.2010.09.010
